Editorial by Βy Prof. Daniele Regge, Chief of the Radiology Unit, Candiolo Cancer Institute (FPO)
The Clinical Vision of the project and added value for patients
One man in eight is diagnosed with prostate cancer during his lifetime and among them, approximately one in 7.5 will die from the disease. To detect prostate cancer, men are invited to perform PSA, usually after the age of 50-55. Unfortunately, PSA has a high rate of false positives, leading to an unnecessary number of second-level investigations, including biopsy.
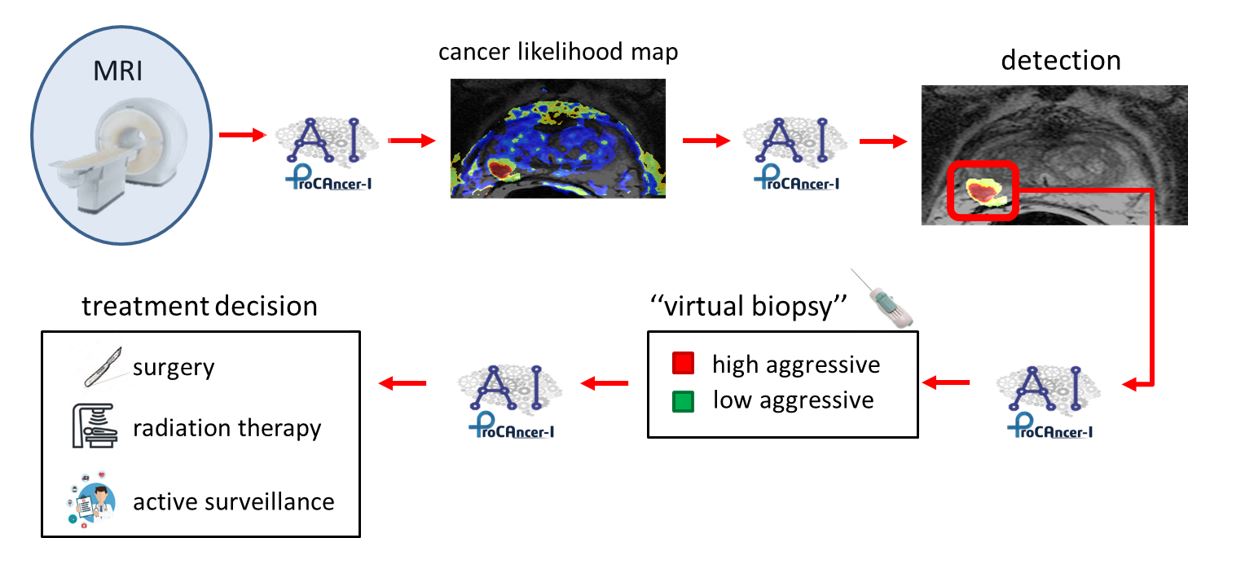
To improve diagnosis, since 2020 urological guidelines recommend Magnetic Resonance Imaging (MRI) because of its high accuracy in detecting clinically significant cancer lesions, i.e. those that need treatment. Moreover, when MRI detects cancer, it provides urologists with information on tumour spatial localization allowing accurate targeting and reduction of the number of retrieved samples, thus limiting procedure-related complications. MRI would be even more beneficial if it could classify lesions according to their risk of progression, a sort of “virtual biopsy” since in this case biopsy could be entirely avoided. The second important reason for performing MRI is that when small-size, low-risk lesions are detected, patients could avoid treatment and undergo follow-up. Indeed, MRI could monitor patients signaling if lesions are turning more malignant.
Unfortunately, MRI provides a visual, necessarily limited, subjective interpretation, which is strongly affected by radiologist experience. Moreover, there is an increasing demand for MRI examinations following the implementation of the new guidelines which is not currently balanced by an adequate number of facilities and dedicated staff.
The vision of ProCΑncer-I, an EU-funded project involving more than 20 research partners across Europe, is to support radiologists, and other clinicians, with state-of-the-art artificial intelligence (AI) MRI-based algorithms with the aim of improving diagnosis and treatment in prostate cancer patients.
Above all, AI tools developed within the consortium aim at distinguishing tumours that are born to be good, requiring no treatment, from those that are born to be bad. The latter grows over time, disseminates, and transforms into a deadly disease. Moreover, ProCAncer-I seeks to predict which cases will metastasize, which could relapse, or which are suitable for active surveillance programs. Knowing which patients are likely to relapse or develop metastatic disease will guide the clinical decisions, optimising the choice of treatments, planning close follow-ups if necessary, and possibly minimising treatment toxicity.
ProCΑncer-I results will bring medicine from the era of “sick care”, in which patients are cured because they have symptoms, to that of “prevention”, where lesions are found and treated before they can grow and become aggressive. This will be possible using AI, which can perceive information in medical images such as MRI, that is hidden from human perception, and give them value.